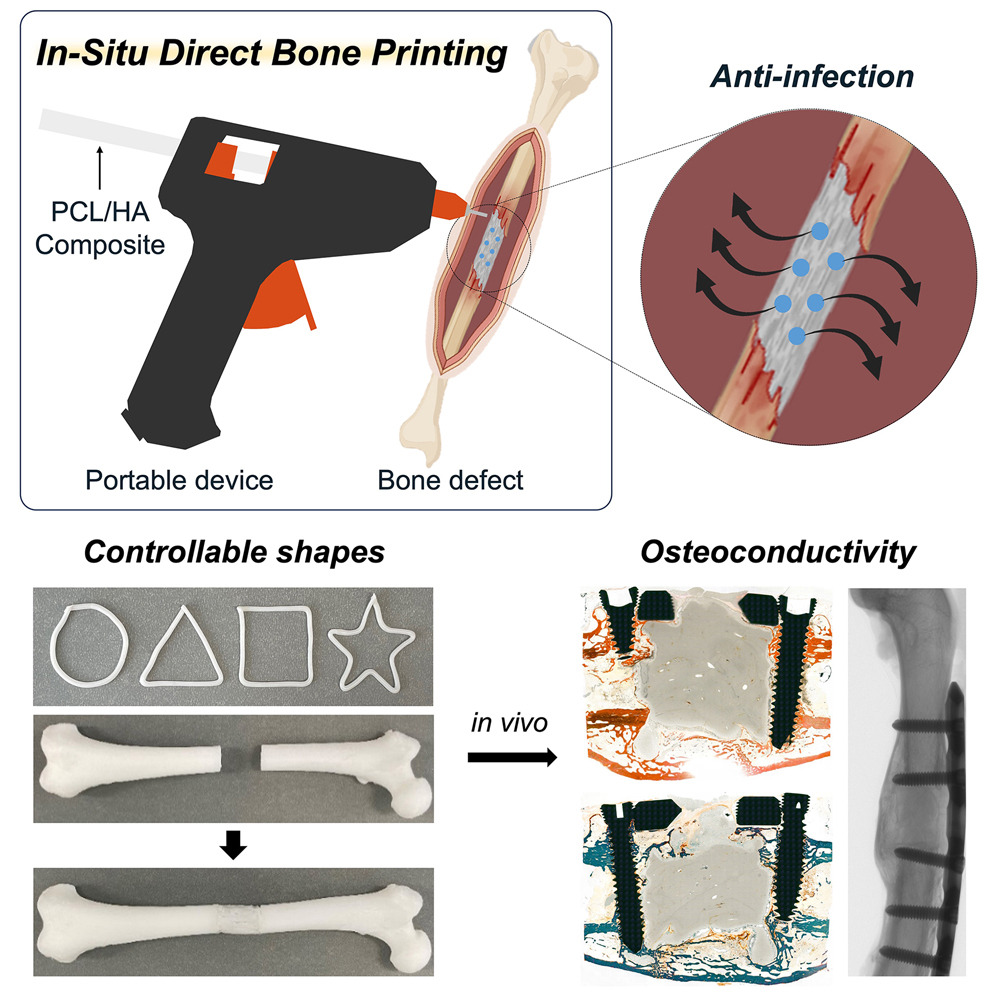
Researchers at Sungkyunkwan University have innovatively modified a common hot glue gun to aid in bone repair. This tool uses a biodegradable glue to mend bone voids quickly and efficiently during surgery. By adapting existing technology, they offer a promising and cost-effective approach to treat various bone injuries promptly.
The Science Behind the Modified Hot Glue Gun
The modified hot glue gun for bone repair represents a revolutionary approach in medical technology, adapting common tools for critical surgical applications. Understanding the science driving its effectiveness involves delving into biomaterials and engineering processes that enhance bone healing.
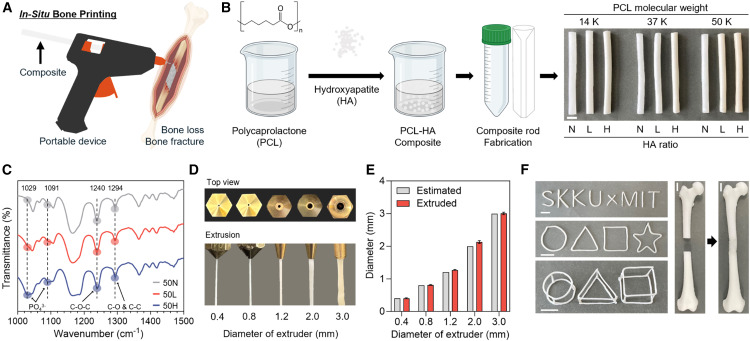
At the core of the glue gun’s success are specialized materials—hydroxyapatite (HA) and polycaprolactone (PCL). Both are vital for bone repair, working synergistically to foster cellular activity and structural integrity in damaged bones.
**Hydroxyapatite** is a naturally occurring mineral form of calcium apatite, one of the primary components of bones and teeth. Its biological significance is astonishing; HA is osteoconductive, meaning it supports the growth of new bone cells by acting as a scaffold. In the modified glue gun, HA acts similarly, guiding bone cells to precisely where they’re needed. Its chemical composition is similar to human bone, which minimizes the risk of rejection and accelerates integration within the body.
**Polycaprolactone**, on the other hand, is a biodegradable polymer that degrades over time without leaving harmful residues. Its role in the modified glue gun is crucial: it acts as a binder that holds the HA particles together while providing flexibility and strength to mimic the properties of natural bone. PCL’s degradation allows for gradual stress transfer to the growing bone, strengthening the site as healing progresses.
The interplay of HA and PCL revolutionizes the application. Together, they create a material strong enough to replace and support bone structures immediately post-surgery, yet intended to degrade as the natural bone restores itself. This synchronization supports physiological processes, ensuring that bone healing occurs efficiently and effectively.
The safe application of these composites during surgery is another significant aspect. Traditional hot glue guns operate at temperatures too high for use in biological contexts, which would destroy delicate tissues and proteins. However, modifying the glue gun to reduce its application temperature addresses this challenge. The gun operates at a lower, controlled temperature, retaining the material’s viscosity necessary for manipulation while ensuring it does not damage the surrounding biological tissues. This refined temperature control is crucial, allowing surgeons to apply the composite directly to affected areas without delays or complications associated with pre-molding or pre-cooling procedures.
The significance of using a biodegradable material like PCL cannot be overstated. As the PCL degrades, the HA becomes more prominent in the matrix, ensuring that as the material’s support wanes, the biological processes take over. This transition taps into the body’s natural healing processes, encouraging proliferation of bone cells and, crucially, the formation of vascular networks. These networks are essential for nutrient delivery and waste removal, supporting long-term health of the newly formed bone.
Moreover, HA and PCL composites foster a biomimetic environment. This setting not only supports osteoblast activity but promotes chemotactic responses, drawing necessary cells and factors to the repair site. This targeted cellular response is invaluable in enhancing healing speeds. Furthermore, the biodegradables used can interact with bone cells on a molecular level, encouraging adhesion, proliferation, and differentiation. This interaction involves the modulation of pathways such as those driven by osteogenic proteins that are critical in new bone formation.
The application of this technology illustrates innovation based not only on functionality but deeply rooted in a comprehensive understanding of biological responses to material properties. The combination of HA and PCL offers a framework that isn’t just structurally complementary to bone, but enhances physiological activities that underpin repair.
Furthermore, the system is adaptable, with potential for surface modifications that enhance specific cellular interactions. For instance, adding nano-scale features to the composite surface can increase surface area and promote even more significant interactions with cellular structures. Such modifications can tweak how cells perceive the material, potentially enhancing outcomes in challenging repair scenarios.
Bringing this modified glue gun to surgical theatres means that we’re seeing a shift in how perioperative care is managed, especially in potentially life-threatening cases. It also opens up new research pathways for integrating biological growth factors or antibacterial agents directly into the material, which could prevent infection at the repair site, a common complication that hinders bone healing.
The modified hot glue gun’s application represents a confluence of materials science, mechanical engineering, and biological understanding, presenting a captivating glimpse into modern medical advancements. These advancements are expanding the possibilities for emergency trauma care, bringing a commonplace, well-understood tool into a domain where intuitive use can significantly impact surgical outcomes. Through strategic modification and material selection, the tool not only offers point-of-care applications but encourages expanding research into complementary materials and technologies that work harmoniously with the human body.
For those intrigued by material science in innovative applications, exploring the potential of biodegradable materials in medical contexts offers rich insights. Discover more about related scientific developments in biomedical materials at a resource like the page on Pi-conjugated Carbon Nanobelts. Such literature provides a more profound understanding of material applications across various fields, highlighting the transformative potential of seemingly simple modifications.
Advantages Over Traditional Methods
The modified hot glue gun method for bone repair presents various advantages over traditional surgical techniques. One of the most significant benefits is the considerable reduction in the time required for the procedure. In emergency trauma situations, time is of the essence. Traditional bone repair methods, such as the use of metal plates and screws, can be time-consuming. Moreover, these methods often necessitate a significant surgical setup and extensive operative time for securing the metal onto the fractured bone.
In contrast, the modified hot glue gun method allows for rapid deployment. Upon application, the biodegradable composite solidifies quickly, providing immediate support to the bone structure. The glue gun, designed with temperature controls, enables surgeons to monitor and apply the material efficiently. This rapid application significantly reduces time in the operating room, which can be crucial in trauma care when every second counts.
Compared to the emerging technique of using 3D printed scaffolds for bone repair, the modified hot glue gun offers even greater time-saving benefits. While 3D printing allows for custom-fit solutions, the preparation and printing of the scaffold can take several hours. This delay may be impractical during emergency situations where rapid intervention is vital. The modified hot glue gun provides a ready-to-use solution that can be applied almost instantaneously.
Additionally, 3D printed scaffolds require specialized equipment and expertise, limiting their availability to major medical centers. The modified hot glue gun, on the other hand, is fundamentally a household tool, albeit highly modified for medical use. Its ubiquitous nature implies that it could be more accessible even in resource-limited settings. This accessibility can prove essential in situations where traditional surgical equipment and materials are unavailable or scarce.
From a financial perspective, the cost implications of the modified hot glue gun are noteworthy. Traditional bone repair materials, like metal plates and screws, come with high manufacturing and material costs. These are further compounded by the costs of sterilization, hospital time, and potential post-operative complications due to hardware rejection.
The modified hot glue gun reduces these costs through several avenues. First, the tool itself, being simple and based on a common device, is inexpensive to produce and maintain. The materials used, such as hydroxyapatite and polycaprolactone, are cost-effective compared to metals and provide the added advantage of biodegradability. This biodegradability reduces the need for secondary surgeries to remove non-degradable materials, thereby minimizing the overall healthcare costs.
Moreover, the potential to integrate antibacterial compounds into the glue gun’s application process offers an additional advantage over traditional methods. Infection is a significant risk in bone surgeries and can complicate recovery and increase healthcare costs. By embedding antibacterial agents within the bone repair material, the modified hot glue gun provides a dual function: bone support and infection prevention. This integration is not only innovative but addresses a critical complication in orthopedic surgeries, enhancing patient recovery and reducing the incidence of post-operative infections. The inclusion of these compounds could be game-changing in improving outcomes in surgical procedures.
Accessibility and cost-effectiveness also play a pivotal role in the broader availability of the modified hot glue gun for bone repair. Owing to its simplicity and the reduced need for high-cost infrastructure, it holds potential for wider implementation in various healthcare settings. Thus, it serves as an equitable solution in both high-tech urban hospitals and under-resourced rural clinics, potentially democratizing surgical care access.
Integrating this tool into the existing healthcare framework may streamline operations and reduce reliance on more intricate and costly equipment. This shift would enable practitioners to focus on delivering care rather than grappling with the limitations of traditional methods—especially in strained medical systems.
The potential impact of incorporating the modified hot glue gun method extends beyond mere efficiency savings. The reduction in operation time can translate to higher throughput in surgical centers, liberating valuable resources, and allocating them to other critical patient care areas leveraging enhanced efficiency.
Furthermore, this approach encourages more sustainable medical practices by minimizing the ecological footprint associated with producing and disposing of metal surgical implants. The biodegradable nature of the materials used ensures that they naturally integrate with the body, reducing environmental waste linked with healthcare.
Embedded within this innovative tool’s framework is the possibility of further technological advancements. Adjustments and refinements could thrive under such a scalable and adaptable model. One can envision enhancements like peripherals that assess the extent of fracture alignment or the emergence of even more sophisticated materials imbued with growth factors or stem cells to accelerate bone regeneration further.
Given the potential for enhanced accessibility and cost reduction, the modified hot glue gun represents a considerable leap forward in orthopedic surgical methods. Ongoing developments and clinical trials will likely cement this tool’s utility, ensuring it becomes an indispensable part of the surgeon’s repertoire.
Alongside the acceleration of recovery times, including features that enhance patient adherence and outcomes, such as the potential integration with wearable monitoring technologies, remains a compelling area of future exploration. This new frontier promises a profound evolution of the surgical landscape toward tailored, patient-centric solutions.
In summary, the modified hot glue gun offers myriad advantages over existing traditional and modern scaffold methods. Its speed, cost-effectiveness, accessibility, and innovative infection-control capabilities underpin its potential as a transformative solution in the realm of emergency trauma and orthopedic care. As healthcare systems continue to prioritize efficient and equitable patient care, such innovations could pave the way for new standards in global bone repair practices.
Future Prospects and Challenges
The modified hot glue gun technique for bone repair holds promise for transforming medical procedures. Its potential extends across various medical scenarios, from battlefield injuries to complex surgical interventions. While this technology seems promising, its path to becoming a mainstream practice faces several challenges. The technology’s future applications and associated hurdles warrant a closer examination.
Potential future applications of the modified hot glue gun technique in medical scenarios are extensive. Its portability and ease of use make it a promising tool in emergency settings, military applications, and austere environments where traditional medical equipment is unavailable. Imagine scenarios where soldiers sustain fractures on the battlefield. Rapid stabilization using a portable and effective method could save lives by allowing for quick evacuations. Furthermore, in remote areas where access to comprehensive surgical facilities is limited, this approach can be a game-changer.
Hospitals are constantly looking for ways to minimize costs and optimize resource usage. The modified hot glue gun provides an affordable alternative to expensive bone grafts or fixation devices. Its ability to integrate antibacterial compounds also promotes faster healing and reduces infection risks. Consequently, hospitals could deploy this technology in both routine surgical procedures and complex trauma recoveries, enhancing patient outcomes while managing operational costs effectively.
The challenges on the path to widespread adoption of this technology are significant and multifaceted. One of the primary hurdles is the need for rigorous clinical validation. The technique must undergo extensive testing to ensure its safety, efficacy, and reproducibility across a wide range of medical scenarios. Large-scale clinical trials involving diverse patient populations would be necessary to establish robust evidence supporting its viability.
Regulatory approval presents another formidable obstacle. Medical devices and procedures require clearance from regulatory bodies such as the FDA in the United States or the European Medicines Agency in Europe. Securing approvals involves demonstrating that the technology meets stringent safety and efficacy standards. This process can be time-consuming and costly, potentially delaying the technology’s entry into the market.
Expert critiques contribute valuable perspectives on the feasibility of this method becoming mainstream. Figures like Benjamin Ollivere emphasize the need for caution and robust evidence before embracing any novel medical technology. Skeptics point out issues such as the strength and durability of the hot glue gun’s adhesive properties compared to traditional methods like metal plates or screws. Additionally, questions about the long-term outcomes of patients treated with this method remain unanswered. Addressing these critiques is crucial for building confidence among healthcare providers and patients.
Technological hurdles must also be addressed for global adoption. Modifying a common household tool for medical use requires precision engineering and rigorous standardization. These modified devices must be tailored to meet the varying requirements of different surgical situations, whether in terms of temperature control, adhesive properties, or sterilization protocols. Research and development efforts would need to focus on perfecting these modifications to ensure consistent and reliable performance.
Training medical personnel in this new technique is another critical aspect. Surgeons and emergency medical technicians must receive comprehensive education and hands-on training to effectively utilize the modified hot glue gun. Developing standardized training programs and integrating the technique into medical curricula can facilitate its acceptance and adoption. Educational institutions and healthcare organizations will need to collaborate to ensure that professionals are well-prepared to implement this method safely and effectively.
While these challenges are significant, the potential benefits of the modified hot glue gun approach make further research worthwhile. Innovations often face skepticism and resistance before acceptance—a pattern seen in countless medical breakthroughs. History is filled with examples of technology that initially seemed implausible but eventually revolutionized healthcare practices. The key lies in addressing concerns seriously and transparently, with a commitment to patient safety and improved health outcomes.
Innovators must continually engage with critics and experts during the research and development process. By incorporating constructive feedback and refining the technology accordingly, developers can overcome barriers and build trust within the medical community. Collaboration across disciplines, from engineers to medical professionals to regulatory bodies, is essential for bridging the gap between innovation and practical application.
Further exploration into the technology’s potential could examine its applications beyond bone repair. For instance, the adhesive properties of the modified hot glue gun may extend to soft tissue repair or wound closure. Researchers might explore how advancements in biomaterials or nanotechnology could enhance the product’s capabilities. Exploring these avenues could reveal new and unexpected benefits, further solidifying the technology’s place in modern medicine.
In conclusion, while the modified hot glue gun method for bone repair faces considerable challenges on its path to widespread adoption, its potential benefits are too significant to ignore. Addressing the hurdles surrounding clinical validation, regulatory approval, expert skepticism, technological development, and training is crucial. By doing so, this innovative approach can move closer to becoming a near-universal tool in medical practice, profoundly impacting patient care and expanding the possibilities for future medical technologies.
Final words
The modified hot glue gun presents a groundbreaking approach to bone repair, combining speed, efficiency, and cost-effectiveness. While it may not replace current methods entirely, it provides a viable alternative for emergency procedures. The integration of antibacterial compounds enhances its potential, offering new insights and opportunities in medical technology for bone healing.
References
In situ printing of biodegradable implant for healing critical-sized bone defect